A Complete Guide to Surrogacy Embryo Transfer
Almost all modern day surrogates are gestational carriers, meaning they get pregnant through IVF fertility treatments. The embryos are created in a lab with sperm and egg from either the parents or donors. The key takeaway is that the surrogate has no biological connection to the baby. She is just the oven, and it’s not her bun.
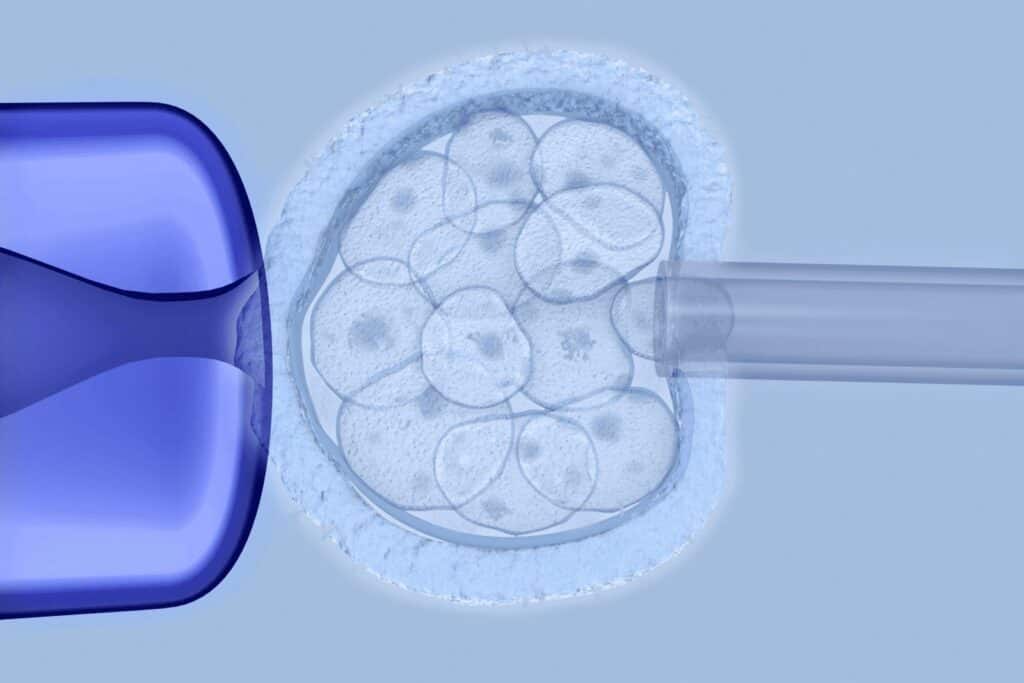
The embryo transfer procedure is the final step of an IVF cycle. This process involves the transfer of an embryo (or more) from a culture dish in the IVF laboratory directly to the uterine cavity. Though each clinic has its own protocols in place for embryo transfers, this guide will help explain:
- How to prepare for an embryo transfer
- What to expect during the embryo transfer
- Tips for after the transfer and during the two week wait
Embro Transfer Preparation
In order for an embryo to implant into the uterus, its lining (endometrium) must be receptive and thickened with blood vessels and nutrients. During a normal menstrual cycle, the hormones estradiol (E2) and progesterone (P4), which are produced by the ovaries, travel to the uterus and cause endometrial thickening in preparation for embryo implantation.
Your embryo transfer cycle begins at the start of your menstrual cycle (cycle day 1), though some women administer medications prior to the start of their menstrual cycles. At the start of your cycle, a fertility specialist will perform baseline monitoring. This monitoring often consists of an ultrasound examination, which ensures that your uterine lining is thin (as it should be at this point the menstrual cycle), and bloodwork, which determines if your hormone levels are within normal ranges.
Medicated vs Natural Transfer Cycles
Many embryo transfer cycles are medicated, meaning that medications are administered to prevent egg maturation and ovulation, thicken the uterine lining, and control the timing of the transfer. If the embryo transfer cycle is medicated, daily injections of estradiol (E2) are administered at the start of the menstrual cycle.
These injections are administered for roughly two weeks, at which time another monitoring appointment is often scheduled. At this appointment, an ultrasound is used to measure the thickness of the uterine lining (we aim for >7mm at this time) to ensure that it is responding to the medications. Bloodwork may also be ordered at this appointment, but this is clinic-specific.
If everything looks normal, daily progesterone injections (known as progesterone in oil, or PIO) and/or vaginal suppositories are administered leading up to (and after) the embryo transfer. The transfer is normally scheduled on the sixth day of progesterone administration if the embryos were frozen 5, 6, or 7 days after they were inseminated.
Some transfer cycles, known as natural transfer cycles, do not require medications and rely on the body’s own hormones to thicken the uterine lining in preparation for the embryo transfer. Natural cycles normally require the same monitoring appointments as medicated cycles, but it is important to know when ovulation occurs during these cycles. This can be determined through ovulation kits, blood work, or ultrasounds. Additionally, a medication can be administered to trigger ovulation to occur. Once ovulation occurs, daily progesterone injections and/or vaginal suppositories are administered in the same manner described above for medicated cycles.
The Embryo Transfer Process
Your IVF clinic will schedule a time for your embryo transfer procedurehttps://alexroblesmd.com/frozen-embryo-transfer-timeline/ and will inform you of when to arrive at the clinic. It’s important to have a full bladder prior to the embryo transfer because it provides a straighter pathway for the catheter and a better ultrasound view.
Embryo transfers are not typically performed under sedation, though some clinics do prescribe Valium prior to the procedure to ease the mind and body. The procedure is minimally invasive and lasts roughly 5-20 minutes.
Before the procedure, you will lie on your back on an exam table with your feet in stirrups. Your fertility specialist will insert a speculum into your vagina to observe your cervix (lower part of the uterus). Once your cervix is in view, your fertility specialist will clean your cervix with a washing solution and insert a catheter through your cervix and into your uterus. The catheter consists of two parts: an outer plastic sheath and an inner flexible “noodle.” The tip of the catheter can be viewed on the ultrasound monitor to ensure that it is in the correct position.
Some clinics load the embryo(s) to be transferred directly into this catheter. If so, the embryo(s) is injected into your uterine cavity once the catheter is in the proper position. Alternatively, some clinics load the embryo(s) into a different catheter (called a replacement catheter). The inner noodle from the catheter inside of your uterus is removed, but the external sheath remains in place. This creates a tunnel for the new noodle with the embryo(s) inside of it. This noodle is then thread through the external sheath from the original catheter and, once it is in position, the embryo(s) is injected into your uterine cavity. You can often see a small flash on the ultrasound screen when the embryo(s) (and a small amount of fluid) is injected into your uterus.
Afterward, the catheter is flushed out to ensure that the embryo(s) successfully transferred into your uterus. If any embryos are retained, the process is repeated. This should not affect implantation rates. Once it’s confirmed that the embryo(s) was successfully transferred, the procedure is complete.
Tips for After the Embryo Transfer Procedure
It was once believed that women had to lie on their backs for ~30 minutes after an embryo transfer to give the embryo time to settle into the uterus. However, studies have found the same success rates when women do not do this. Therefore, most clinics will release you shortly after the procedure is over.
Your fertility specialist will review your rules and restrictions before you leave the clinic. Though each specialist has his/her own set of rules and restrictions that you should abide by, common rules and restrictions often include:
- Do not physically or mentally overexert yourself. Try your best to relax and avoid stressors (like social media).
- Maintain a healthy balance of resting and walking. This helps improve blood circulation but prevents overexertion.
- Do not smoke, drink alcohol, or engage in recreational drug use.
- Avoid hot tubs or baths.
- Drink a lot of water to avoid dehydration.
- Continue administering progesterone unless otherwise indicated.
- If you have not already, begin taking a prenatal vitamin.
- Avoid intercourse, which can cause uterine contractions.
While most women are cleared to return to work the day after an embryo transfer, some women prefer to take the following day off from work. This is a personal preference that can be discussed with your fertility specialist after your embryo transfer.
Post-Procedure Pregnancy Tests
Most fertility clinics will schedule a clinical (quantitative) pregnancy test 9-12 days after the embryo transfer is performed. This test measures the level of hCG (human chorionic gonadotropin, a hormone produced by cells in the placenta) in the blood. If there is an adequate amount of hCG in the blood, it confirms that embryo implantation occurred.
In these cases, bloodwork is repeated 1-2 more times over the course of a few days to ensure that the hCG levels are rising appropriately (we hope to see the levels double every other day). After multiple normal results, an ultrasound is normally scheduled to observe the gestational sac and fetal measurements.
Home Pregnancy Tests
The two week wait can be a difficult time for surrogates and their intended parents. It is okay to feel anxious and excited, but too much stress can actually harm the process. Though it is tempting to take a home pregnancy test, it is advised to wait for a blood test to confirm a pregnancy. At-home tests can cause a lot of unnecessary stress and cannot always detect hCG before a scheduled blood test.
Being that I personally know a lot of surrogates, the home pregnancy tests are kinda a “thing” and quickly show-up on social media videos. My advice is if you really want to take the home tests, make sure your intended parents are okay with it. Secondly, don’t share anything publicly until you have the confirmed blood work done. Lastly, know that early negative and positive results are not the actual results. You can get false negative results because the hCG levels are not high enough, and you can get false positive results from a “chemical pregnancy.”
It is recommended to use this time to:
- Binge watch a TV show.
- Catch up with a supportive friend or family member over lunch or a walk around a park.
- Read a series of books (just for fun!).
- Practice relaxation techniques such as meditation with positive manifestation mantras.
What if I Have a Failed Embryo Transfer?
There are many factors that determine one’s chance of success following an embryo transfer. It’s important to remember that, even after a perfect embryo transfer, a successful outcome is not guaranteed. If your first embryo transfer is not successful, it does not mean that a subsequent transfer will also be unsuccessful. If this occurs, talk with your doctor about the possible causes of the failed cycle and what changes can be made during a future embryo transfer.
The embryo transfer procedure is an exciting step in one’s fertility journey, but it can also be a mentally and emotionally stressful period of time. If you are experiencing extreme feelings, please contact your fertility specialist or another medical professional for assistance.
About the Author
Jessica Manns is an experienced embryologist and the creator of Explaining IVF. She obtained her Bachelor of Science from the University of Pittsburgh in 2016 and her Master of Biomedical Science from Colorado State University in 2018. Since that time, Jessica has achieved her dream of becoming an embryologist and helping others build their families. In addition to her career as an embryologist, Jessica launched her social media platform, Explaining IVF, in 2022 to educate the public about IVF and infertility. She has also written a number of informative blog posts, guest starred on multiple podcasts, and hosted/co-hosted various Instagram Live events, all of which pertain to IVF and infertility. Jessica helps lead a local infertility support group in Pittsburgh, PA, and thoroughly enjoys helping others through their fertility journeys.
Learn More